Indoor air quality is an important requirement in all buildings, but it is especially critical for hospitals and health facilities. With poor ventilation and various microorganisms that survive and get circulated in the air, hospitals can be hotbeds for harmful pathogens such as the coronavirus.
Healthcare-Associated Infections, also known as HAI or nosocomial infections, are infections that people contract in a healthcare facility while receiving treatment or professional care. Although HAIs are typically referred to as conditions that develop within 48 hours or more after admission or visit to a healthcare facility, studies show that the illnesses can manifest weeks or even months later. These infections are a great risk to all patients who have compromised immunity, as well as the doctors, nurses, staff, and visitors. HAI is a serious health problem not only because it could lead to more deaths but because of its heavy toll on the length of hospitalization, increased healthcare costs, and reduced productivity of healthcare staff. In the US alone, it is estimated that 1 in 21 patients seeking treatment is likely to get HAI that can worsen their disease or in some cases become terminal.
Many of these infections are preventable and understanding the factors that influence them can help to address and manage this public health issue.
Identifying HAI causes and the environment that supports it
HAI can occur in different health care environments, from outpatient care facilities such as health clinics, surgical facilities, dialysis centers to long-term care facilities such as rehabilitation and nursing home centers.
Although there is no conclusive study defining the sources of HAI outbreaks as of yet, continuing research on the matter reveals common patterns. A study by Duke University School of Medicine showed that pathogens can “travel between the transmission triangle in a health care setting” which involves the patients, the environment, and the health care provider. Patients with underlying or preexisting medical conditions are the main source of contaminants in healthcare facilities and not to be overlooked are other equally critical sources which include medical and surgical equipment and devices, contaminated medicines and food, healthcare personnel who have been exposed and carry the pathogens in their system, as well as treatment rooms and facility halls.
In many of these studies, a crucial element found to enable the survival and transmission of these harmful microorganisms is poor indoor air quality. Bacteria and viruses can survive on droplets and can remain airborne indefinitely. With poor air exchange, these pathogens are more likely to spread. This can be exacerbated by occupant density which is a typical occurrence in emergency rooms, waiting areas, or patient wards with multiple beds in a small room. Moreover, if the health care facility’s heating, ventilation, and air conditioning system is not properly maintained, it can be a reservoir for these pollutants.
Assessing the Various Needs for Indoor Air Quality in a Health care setting
Traditional health care facilities such as hospitals have rooms for various purposes calling for different airflow rates and air quality standards. For instance, critical environments such as surgical rooms and burn units require higher air changes per hour (ACH) than inpatient rooms because of the need to dilute and remove concentrations of airborne microorganisms which can cause infections.
A diagram showing requirements that vary per room presents a complex ecosystem.
Here are a few takeaways from this diagram:
- Air pressure, temperature, and humidity requirements can vary from one room to the next.
- Ventilation or the rate of air exchange also varies depending on the purpose of the room.
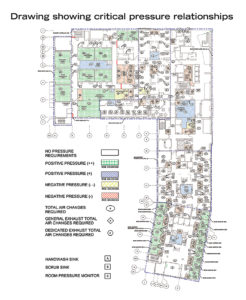
Source: https://www.hfmmagazine.com/
The Role of IAQ management in HAI prevention
Ensuring a healthy hospital can be very challenging. But as the old adage goes, “an ounce of prevention is worth a pound of cure.” The role of healthcare administrators and managers is to understand the relationship between indoor air quality and HAI and what approaches can be taken to manage the risk.
Having real-time visibility on indoor air quality factors can help facility managers to identify environments that face higher risks and allocate adequate resources to implement appropriate approaches to mitigate them. Air quality data can also provide valuable insights that can help in developing a risk management plan which includes proper education and training of health care workers, compliance with, and adoption of best safety and sanitation practices to prevent HAIs.